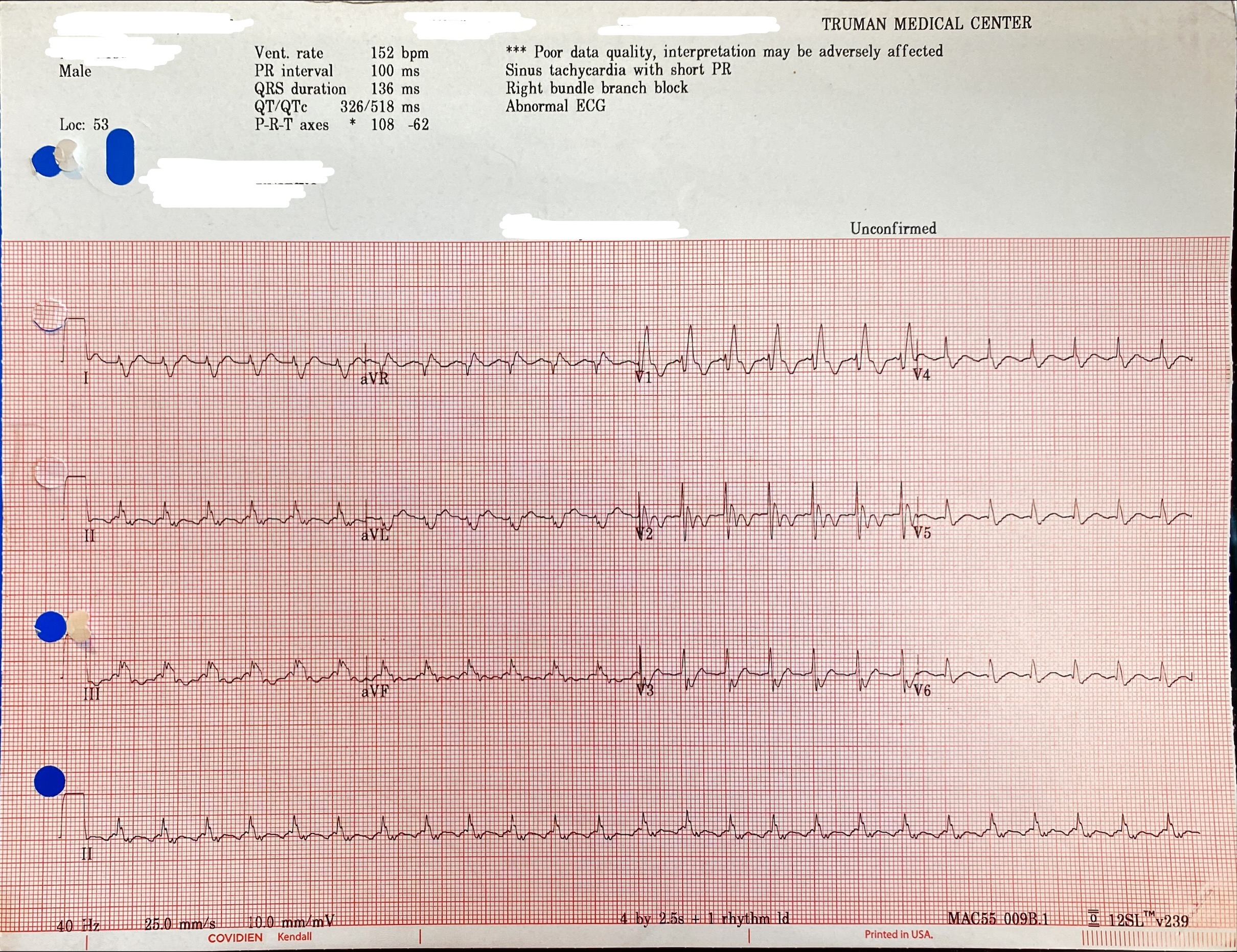
Narrow complex tachycardia from a critically-ill 55-year-old ICU patient shows an old RBBB and which of the following rhythms?
- Sinus Tachycardia.
- Atrial Flutter with 2:1 conduction.
- Atrial Fibrillation.
- AV Nodal Reentrant Tachycardia (AVNRT).
- Atrial Tachycardia with 1:1 conduction
The right answer is:
2- Atrial Flutter with 2:1 conduction.
Explanation:
This is a rhythm that was frequently encountered by multiple residents and can be easily confused with sinus tachycardia or other arrhythmias especially in the background of a critically ill patient. It is one of the most commonly overlooked cardiac arrhythmia — and one of the best ways to never again overlook Atrial Flutter is to always LOOK FOR IT whenever you have a regular tachycardia at ~150/minute without clear sign of SINUS P waves. The differential can always include sinus tachycardia (with P wave buried in the T wave), AVNRT/AVRT, and atrial tachycardia.
Tips for Spotting Atrial Flutter
- Suspect flutter with 2:1 block in any patient with a regular narrow complex tachycardia at 150 bpm (130-170).
- Scrutinize leads II and V1 for flutter waves.
- Flutter waves are typically sawtooth (inverted) in lead II and resemble upright P waves in V1 (Figure 1).
- Vagal Maneuvers +/- Adenosine: AVNRT/AVRT will often revert to sinus rhythm, whereas slowing of the ventricular rate will unmask the underlying atrial rhythm in sinus tachycardia or atrial flutter (transient period of increased AV block during which flutter waves and sawtooth pattern may be unmasked) (Figure 2).
- Try turning the ECG upside down — this can make the flutter waves in lead II easier to see (Figure 3).
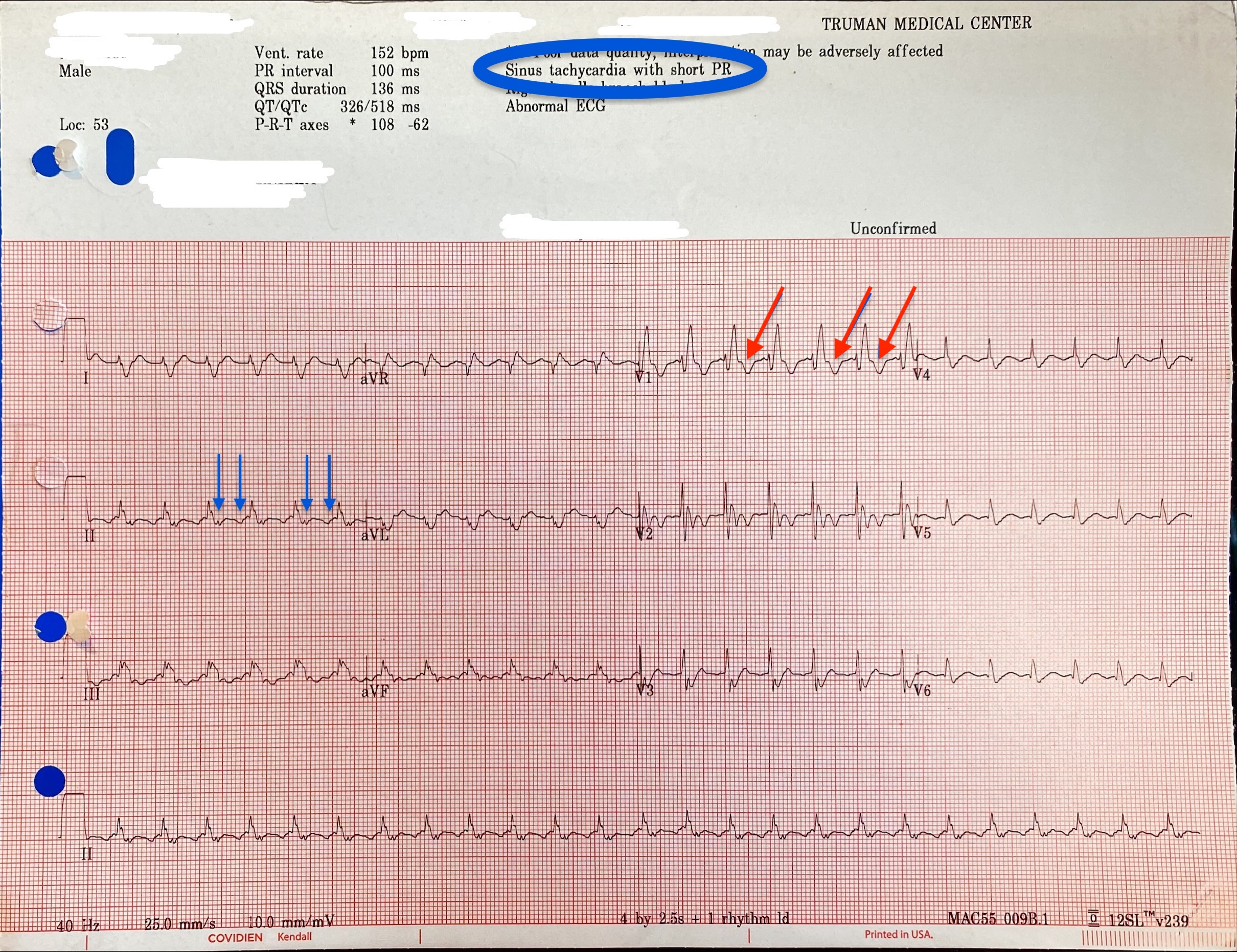
Figure 1: Note how the ECG machine interpretation mistakenly labeled the rhythm as sinus tachycardia. Also, note the inverted flutter waves in lead II (blue arrows). Some may mistakenly think the peak between the 2 inverted waves is a sinus P wave. Also, the upright flutter (resembling P waves) waves were not very clear in this patient in lead V1. However, note the small notch on the beginning of the T wave which corresponds to the first flutter wave between 2 complexes (red arrows).
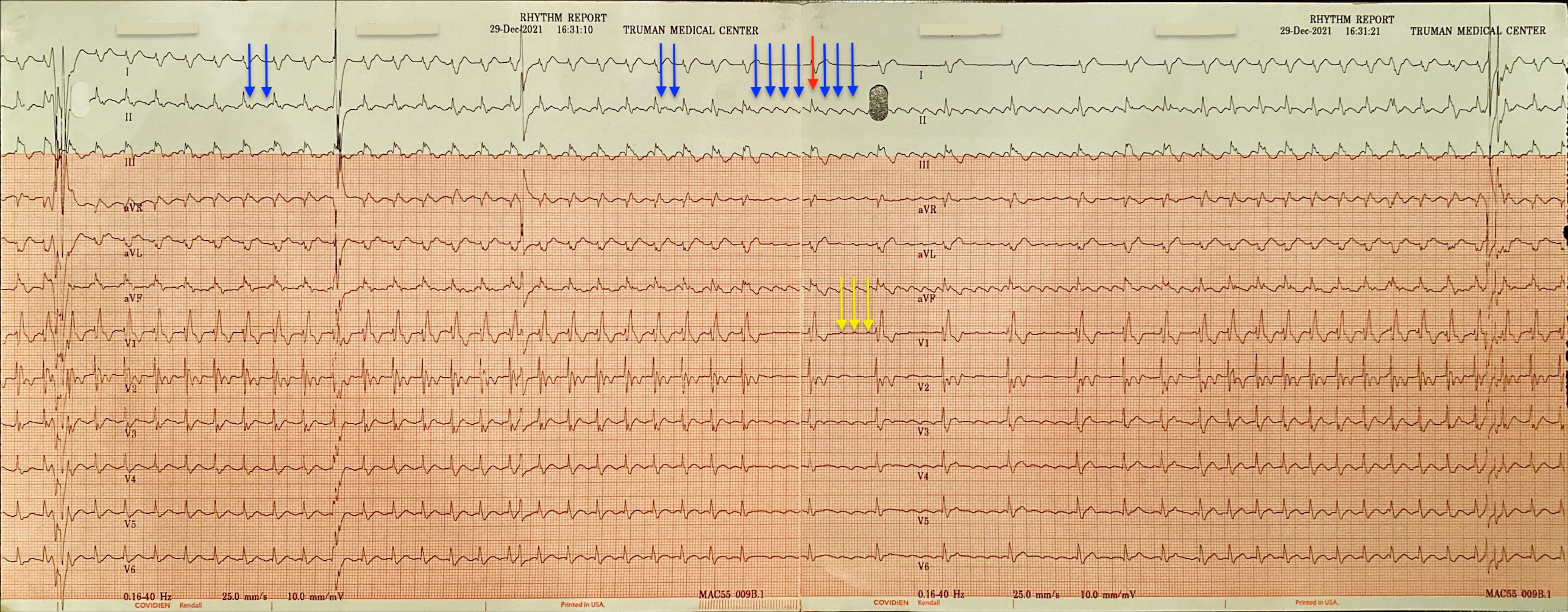
Figure 2: The same patient received adenosine while connecting 12 lead ECG and recording rhythm strip simultaneously. Note how the inverted flutter waves in lead II transform to a sawtooth with the slowing of heart rate (blue arrows) with one wave buried in the QRS complex (red arrow). Also, note the appearance of multiple upright waves resembling upright P waves in lead V1 (Yellow arrows).
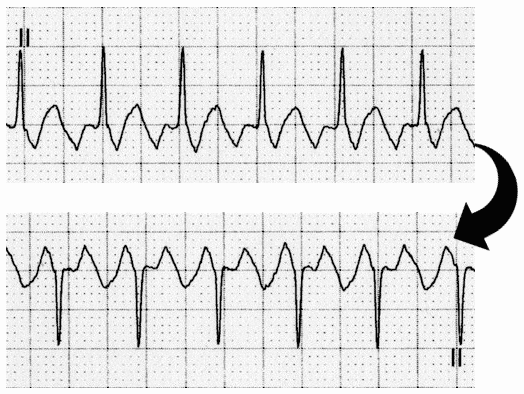
Figure 3: Lead II turned upside down.
Bottom line: ALWAYS suspect atrial flutter whenever you see a fixed rate around 150 (130-170).
Extra food for the brain – pathophysiology, and physics
Atrial flutter is a form of supraventricular tachycardia caused by a reentry circuit within the right atrium. The length of the re-entry circuit corresponds to the size of the right atrium (Figure 4), resulting in a fairly predictable atrial rate of around 300 bpm (range 240-330). In contrast, the rate in sinus tachycardia typically varies slightly from beat to beat, while in AVNRT/AVRT the rate is usually faster (170-250 bpm)
- Ventricular rate is determined by the AV conduction ratio (“degree of AV block”). The most common AV ratio is 2:1, resulting in a ventricular rate of ~150 bpm
- Higher-degree blocks can occur — usually due to medications or underlying heart disease — resulting in lower rates of ventricular conduction, e.g. 3:1 or 4:1 block.
- Atrial flutter with 1:1 conduction can occur due to sympathetic stimulation, or in the presence of an accessory pathway. The administration of AV-nodal blocking agents to a patient with WPW can precipitate this
- Atrial flutter with 1:1 conduction is associated with severe hemodynamic instability and progression to ventricular fibrillation
- NB. The term “AV block” in the context of atrial flutter is something of a misnomer. AV block is a physiological response to rapid atrial rates and implies a normally functioning AV node, not a true heart block The re-entry circuit typically involves the Cavo-tricuspid isthmus (CTI) which provides a well-localized ablation target. CTI ablation creates a scar that interrupts the circuit and prevents further development of atrial flutter (Figure 4).
The re-entry circuit typically involves the Cavo-tricuspid isthmus (CTI) which provides a well-localized ablation target. CTI ablation creates a scar that interrupts the circuit and prevents further development of atrial flutter (Figure 4).
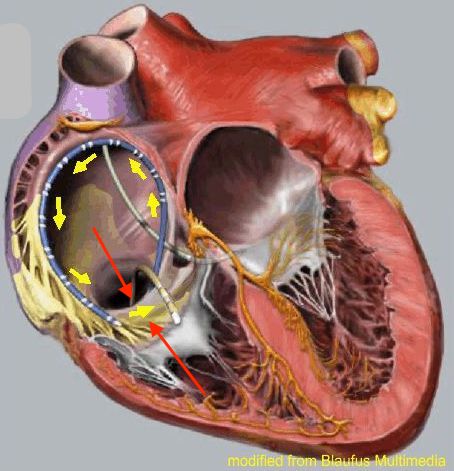
Figure 4: Anatomical path of the re-entry circuit. Disregard the 3 catheters in the diagram. Note that the re-entry circuit has to pass through the narrow conductive tissue (red arrow) between IVC and Tricuspid annulus inferiorly (Cavo-tricuspid isthmus) to complete the circle.
Although atrial flutter most commonly presents with inverted P waves (sawtooth) in lead II, It can present also in different variants. So, the absence of the typical saw tooth even after slowing down the heart rate, doesn’t completely rule out atrial flutter diagnosis. Here’s a brief note on types of atrial flutter:
Typical atrial flutter (Common, or Type I Atrial Flutter)
Involves the IVC & tricuspid isthmus in the reentry circuit. Can be further classified based on the direction of the reentry circuit (anticlockwise or clockwise):
Anticlockwise Reentry: Commonest form of atrial flutter (90% of cases). Retrograde atrial conduction produces:
- Inverted flutter waves in leads II, III, aVF
- Positive flutter waves in V1 – may resemble upright P waves
Clockwise Reentry: This uncommon variant produces the opposite pattern:
- Positive flutter waves in leads II, III, aVF
- Broad, inverted flutter waves in V1
Atypical atrial flutter (Uncommon, or Type II Atrial Flutter)
- Not CTI dependent. Can arise from any location (usually scar related e.g. surgery, ablation,etc)
- Does not fulfill criteria for typical atrial flutter
- Often associated with higher atrial rates and rhythm instability
- Less amenable to treatment with ablation
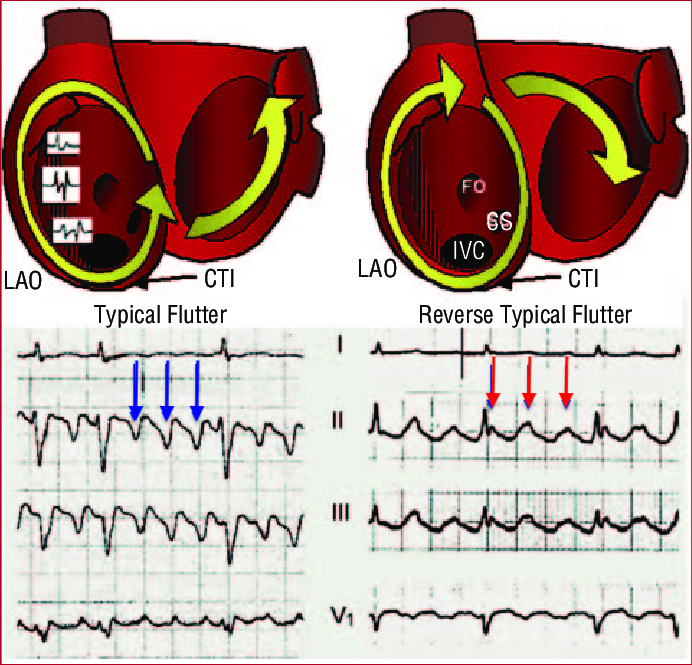
Figure 5: Left: Typical counterclockwise Flutter. Note inverted P waves marked by the blue arrow as the depolarization wave spreads from below upwards (away from inferior leads and thus negative P wave). Right: Clockwise Flutter. Note upright P wave in the inferior leads (II and III) as the depolarization wave spreads from above downwards (toward the inferior leads and thus positive P wave)
Finally, you can check this video for an animated illustration. It shows 3 types of SVT. The last one is atrial flutter. https://www.youtube.com/watch?v=xLzRFAT9uFA
References:
- Goldberger, Ary L., Zachary D. Goldberger, and Alexei Shvilkin. Clinical electrocardiography: a simplified approach e-book. Elsevier Health Sciences, 2017.
- Ed Burns. Life in the fast lane. https://litfl.com/ecg-case-042/
- Wesley Todd. A Flutter. Wes Todd’s blog. http://wesleytodd.blogspot.com/2013/08/atrial-flutter-describe-direction-of.html.
- Atrial Flutter: an Update - Scientific Figure on ResearchGate. Available from: https://www.researchgate.net/figure/Mechanism-and-electrocardiographic-pattern-of-typical-atrial-flutter-left-and-reverse_fig1_6850918 [accessed 30 Jan, 2022]