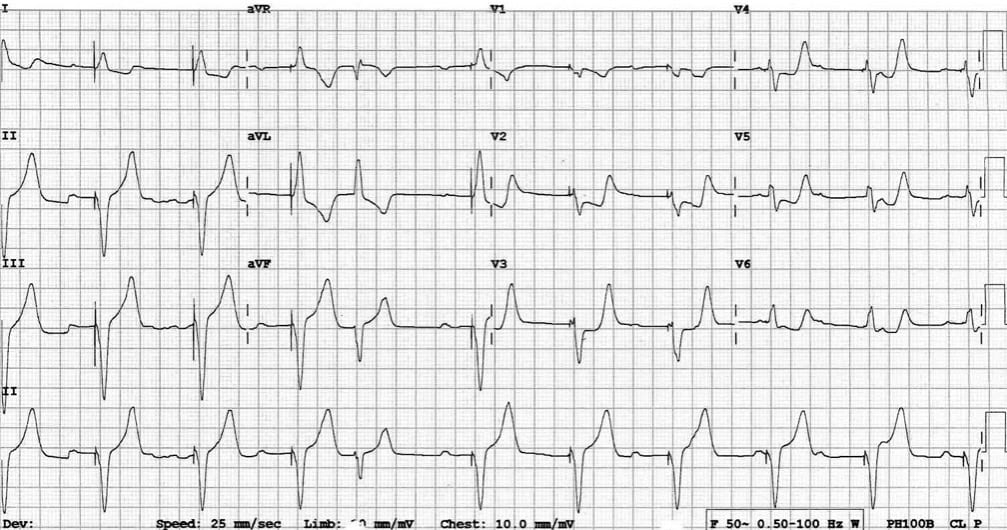
67-year-old with a history of complete heart block and pacemaker placement presenting with chest pain. What is your diagnosis?
- Pacemaker syndrome
- Pericarditis
- Myocardial infarction
- Pulmonary embolism
- Pre-excitation
The correct answer is:
3. Myocardial infarction.
Explanation:
Left Bundle Branch Block (LBBB) and ventricular paced rhythm have an abnormal depolarization pattern and subsequently abnormal repolarization pattern (will be explained further in a future quiz). And as we discussed in quiz 1, a current of injury is usually manifest during the repolarization phase. Hence, a diagnosis of myocardial infarction (MI) made by identifying the typical ST-T changes -in the proper clinical setting- can be challenging in LBBB and ventricular paced rhythm.
You should expect in LBBB and ventricular paced rhythm that repolarization waves are discordant from the depolarization wave, i.e., a predominantly negative QRS complex will be followed by ST elevation and upright T wave. In contrast, a predominantly positive QRS complex will be followed by ST depression and an inverted T wave (Figure 1). Now you understand why it's challenging to recognize MI when ST elevation is actually an expected common finding in LBBB and ventricular-paced rhythm.
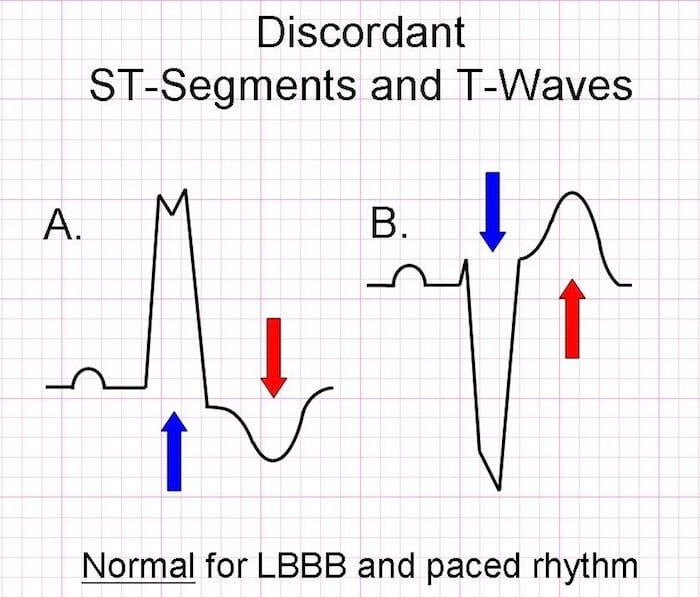
Figure 1: Normal discordant waves in LBBB and ventricular-paced rhythm.
It used to be believed that recognizing a MI in those rhythms can be impossible. In a previous version of the STEMI guidelines, a new -or presumed new- LBBB was treated as STEMI when encountered in the proper clinical setting (a recommendation that was removed from the latest STEMI guidelines).
In the above case, you can always turn off the pacemaker and cross fingers they will still have an intrinsic rhythm to help you recognize ST elevation of MI ... and help them stay alive (it's a joke, you can laugh), or you can search for other less risky ways.
Elena Sgarbossa described a way -back in 1996- to recognize MI in LBBB. Sgarbossa method was then applied for the same purpose in ventricular-paced rhythm. Later on, in 2012, Stephen W. Smith published a modification of the Sgarbossa rule that was validated later on in 2015.
Modified Sgarboss rule (Figure 2):
- Concordant ST-elevation ≥ 1 mm in ≥ 1 lead
- Concordant ST depression ≥ 1 mm in ≥ 1 lead of V1-V3
- Proportionally excessive discordant ST elevation in ≥ 1 leads anywhere with ≥ 1 mm ST elevation, as defined by ≥ 25% of the depth of the preceding S-wave.
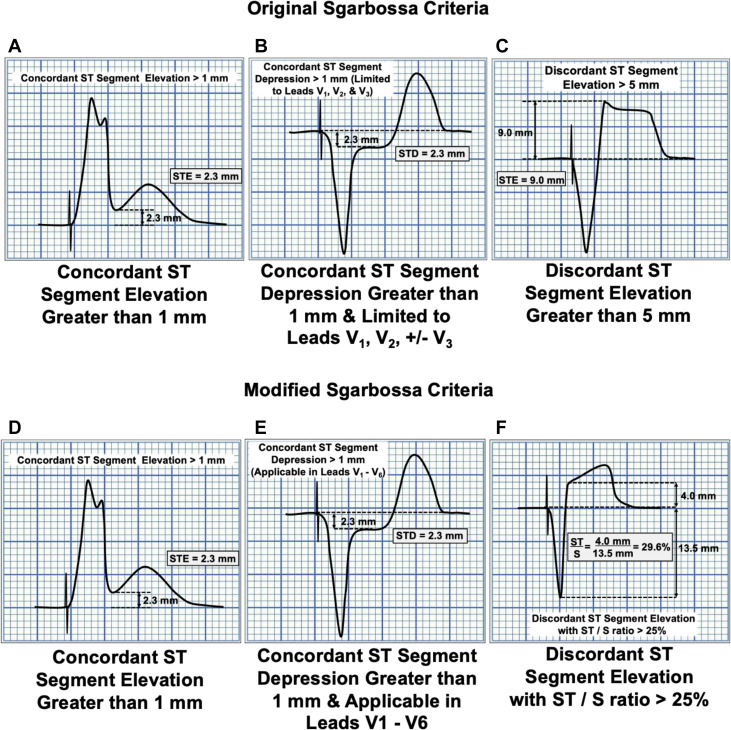
Figure 2: Original Sgarbossa criteria compared to the modified criteria. Note that, in the original criteria, the finding in the C panel takes a score of 2 and is not specific and not diagnostic.
An advantage of the modified Sgarbossa rule is that it's considered positive for MI if any of the three criteria are positive, making it easier to memorize than the original Sgarbossa rule that relied on a scoring system where a low score of 2 was non-diagnostic and not specific.
Our quiz patient had concordant ST depression in V2-5. This violates the expected pattern of discordance for a V-paced rhythm and is a marker of superimposed myocardial infarction. This patient did indeed have an isolated posterior infarction due to complete occlusion of a posterolateral branch of the RCA. She was successfully treated with PCI.
A trick to memorize the criteria:
The way I think about it is this 2x2 table that relies on two facts:
- Discordance is expected in LBBB and paced rhythm and can be normal. Hence, any concordance is "no bueno," while discordance can be anything.
- ST-elevation is always worse than ST depression.
Based on these two pieces of information, I pick the three most dangerous findings from the 2x2 table (Figure 3) and consider MI as a diagnosis if any of them was positive.
- Concordant elevation.
- Concordant depression.
- (Excessive) Discordant elevation
Note that discordant depression was not included, which makes sense as it's the least valuable finding according to the above two facts.
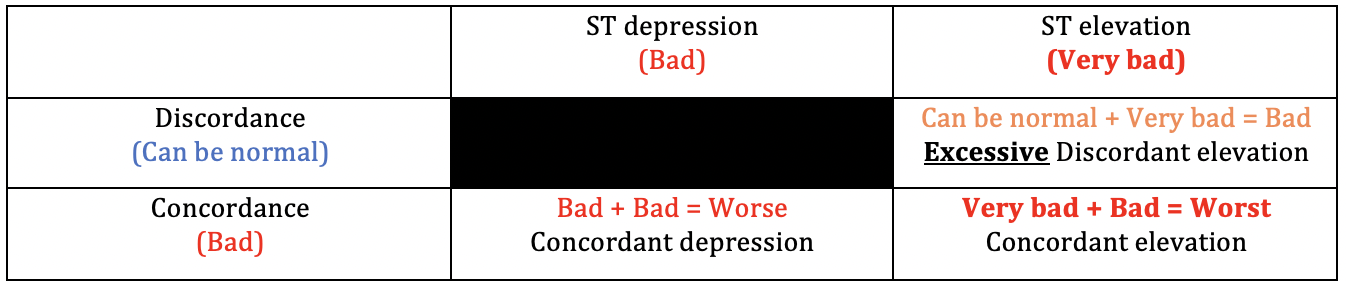
Figure 3: A schematic table to identify the most important findings based on the fact that concordance is always bad and the finding of ST-elevation is worse than depression. The grading from "Bad" to "Worst" helps recognize how to score these findings in the original criteria, which you don't have to know anymore with the new criteria.
Finally and most importantly
- Don't use Sgarbossa criteria to rule out MI. Remember, it's poorly sensitive. But it's specific and can be used to rule it in and guide further management.
- If Sgarbossa criteria are negative in a setting where MI is suspected, continue to repeat ECG, trend troponin, and consider Echo to assess the possibility of MI further.
The following video is a fun one, a song and a very brief interview with Elena Sgarbossa M.D.
And always remember; Sgarbossa criteria: rule in but can't rule out.
References:
- Sgarbossa EB, Pinski SL, Gates KB, and Wagner GS. Early electrocardiographic diagnosis of acute myocardial infarction in the presence of ventricular paced rhythm. GUSTO-I investigators. Am J Cardiol 1996 Feb 15; 77(5) 423-424
- Sgarbossa EB et al. Electrocardiographic diagnosis of evolving acute myocardial infarction in the presence of left bundle-branch block. GUSTO-1. N Engl J Med 1996 Feb 22; 334(8) 481-7
- Smith SW et al. Diagnosis of ST-Elevation Myocardial Infarction in the Presence of Left Bundle Branch Block using the ST-Elevation to S-Wave Ratio in a Modified Sgarbossa Rule. Annals of Emergency Medicine 2012;60:766-776
- Meyers HP, Limkakeng AT Jr, Jaffa EJ, Patel A, Theiling BJ, Rezaie SR, Stewart T, Zhuang C, Pera VK, Smith SW. Validation of the modified Sgarbossa criteria for acute coronary occlusion in the left bundle branch block setting: A retrospective case-control study. Am Heart J. 2015;170(6):1255-1264.