You are seeing a new consult for ventricular tachycardia on telemetry. What's the rhythm?
- Artifact
- Ventricular Tachycardia
- Ventricular Fibrillation
- Atrial fibrillation
- Atrial Flutter
The right answer is:
1- Artifact
Explanation:
Dilemma:
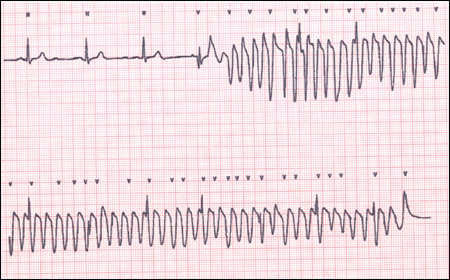
Ventricular tachycardia can be monomorphic (same shape), as seen in figure 1: the ventricular complexes that comprise the ventricular tachycardia are all of the same wide repeating patterns. This appearance is deceptively similar to different types of artifacts (muscular artifact due to movement, eating, seizure, etc.) as seen in figure 2 tracing.
Solution:
There are different keys to expose those tricky telemetry alarms:
- Always look at the patient: are they doing push-ups or sweaty in bed with palpitations? Sounds intuitive, Doesn’t it? You’re probably asking why am I being told this when I should be learning about ECG. The answer is that people frequently miss this small detail. But you’re probably right so let’s move on to point 2.
- Look closely at the deflections in the tracing. It looks wide, bizarre, and not identical like the monomorphic VT in figure 1. Are you thinking maybe because it can be polymorphic tachycardia or V.Fib? I’ll resist saying “go back to point 1 as these rhythms are incompatible with life”, and move with you to point 3 instead.
- Look for interspersed evenly-spaced sharp wave pattern (may not be evenly-spaced if the underlying rhythm is A.Fib.). This is the underlying rhythm with the superimposed artifact (arrows in Figures 2 and 3).
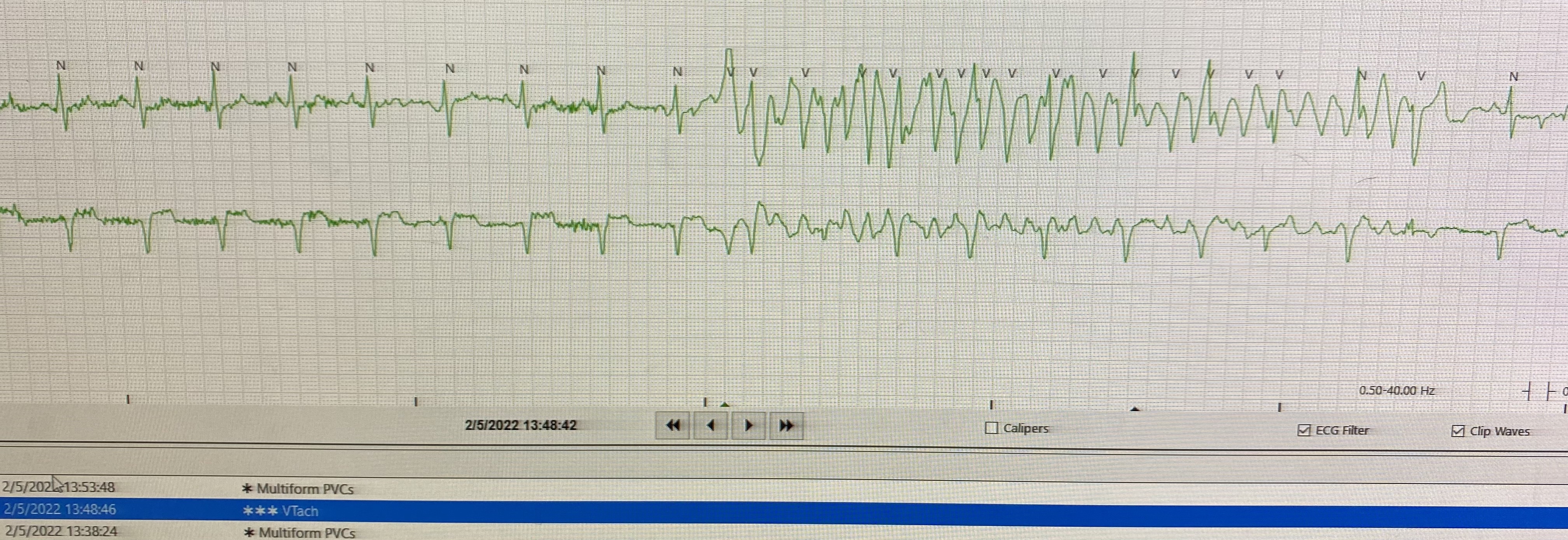
- Examine other leads in the telemetry. The telemetry screen doesn’t usually show all recorded leads instead, they only show one or two leads. There’s a fair chance this artifact is not recorded by other leads and you will be able to see a normal rhythm. Luckily, our patient had extra lead connected showing the normal rhythm (figure 4). That’s right, if there were tachycardia it would have been recorded by all leads.
- Use Calipers (Explained below): start with the last 2 normal beats and march your caliper forward and see if there is a sharp complex where you expect a normal beat in continuation to the normal rhythm preceding the artifact/tachycardia.
- Finally, The presence of unchanged pulse oximetry curves further points towards the presence of artifact.
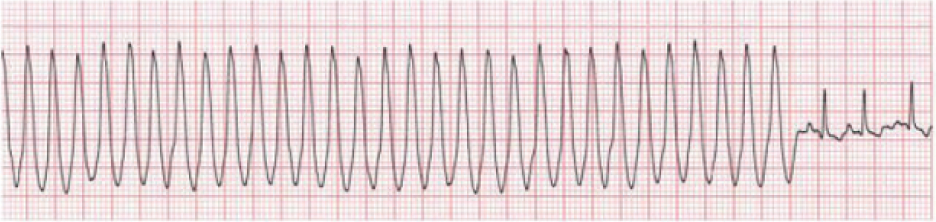
Figure 1: Monomorphic tachycardia.
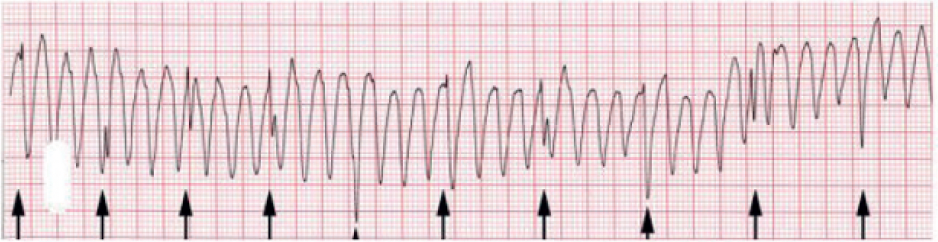
Figure 2: Artifact. Arrows point to the interspersed QRS complexes
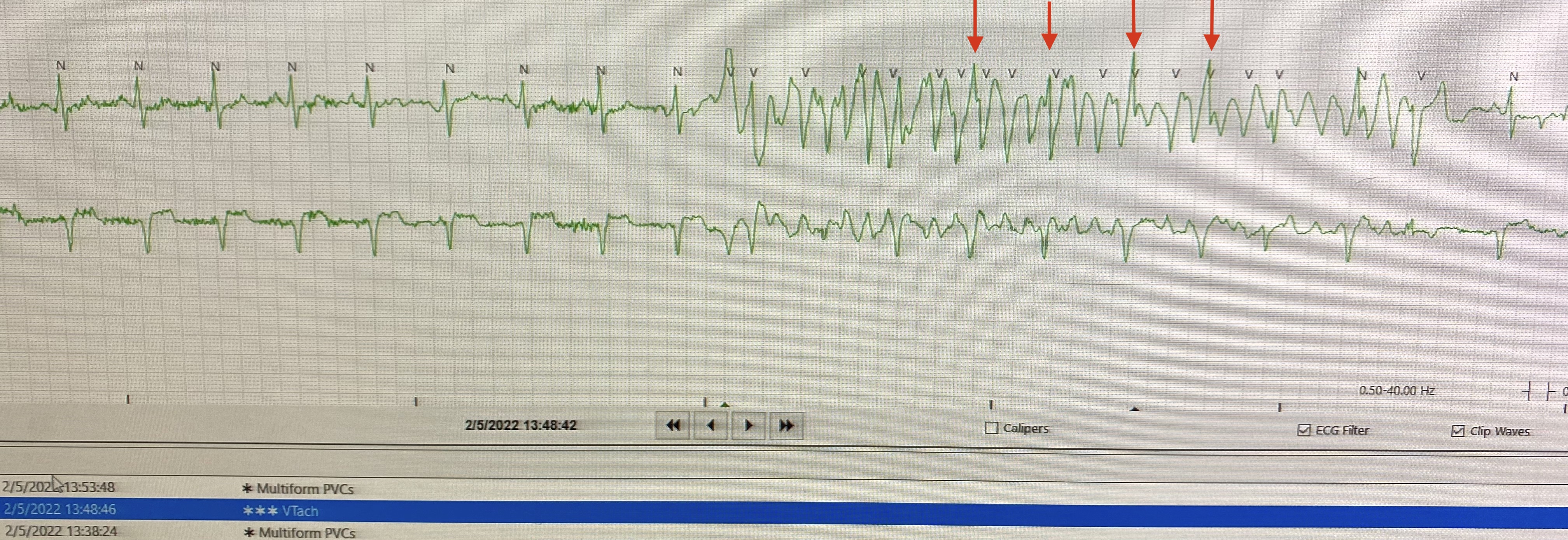
Figure 3: Artefact. Arrows point to the interspersed QRS complexes
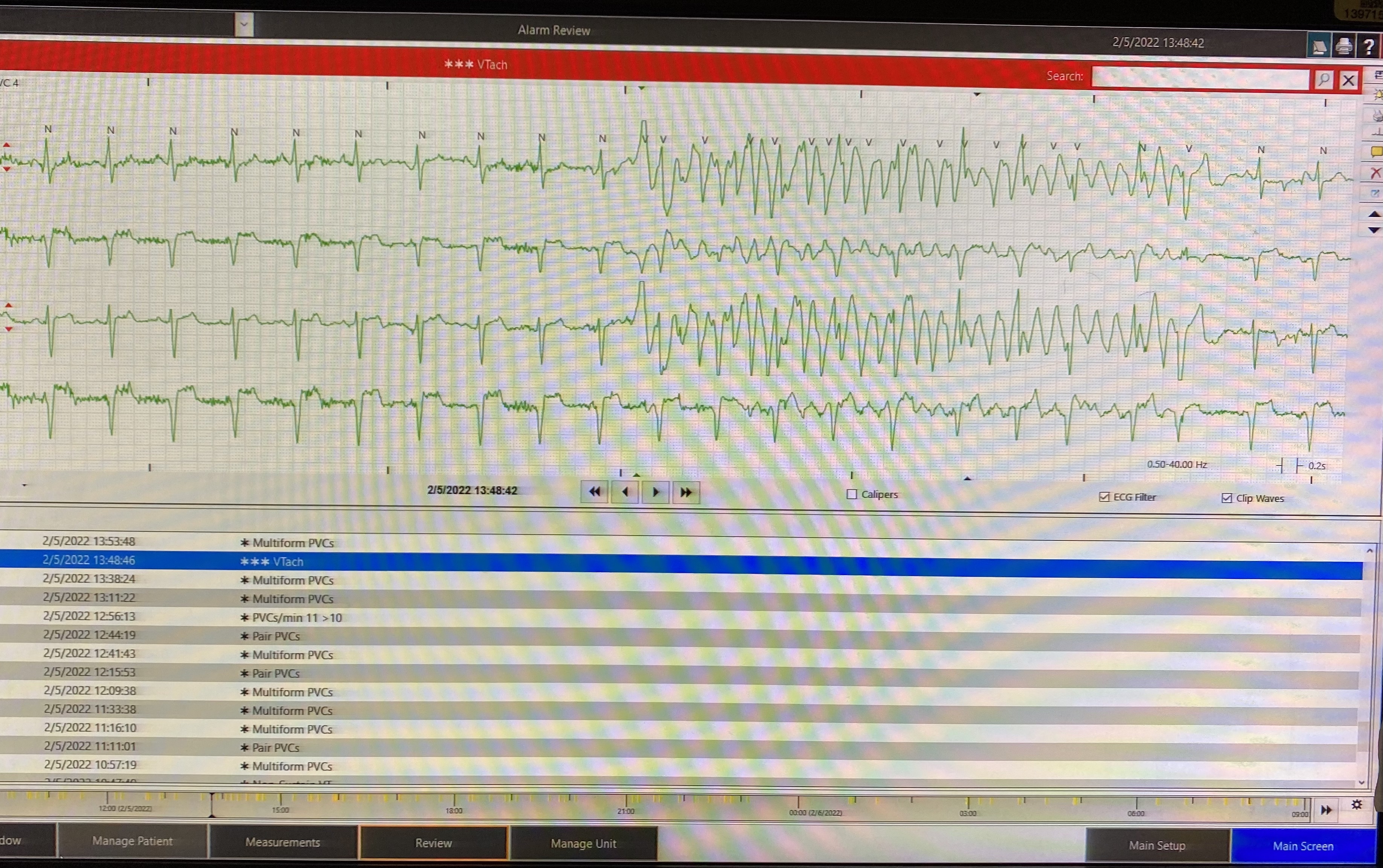
Figure 4: Same patient showing more leads on the telemetry screen. Note the down most lead doesn't show VT.
General Telemetry tricks
A general approach to reviewing telemetry while pre-rounding at SLH:
These are suggested steps for a basic review of telemetry. You might need some extra steps in special cases. You can also develop your own algorithm for reviewing telemetry. There is no right answer.
1- Can start with “alarm review” from the review tab below (figure 5).
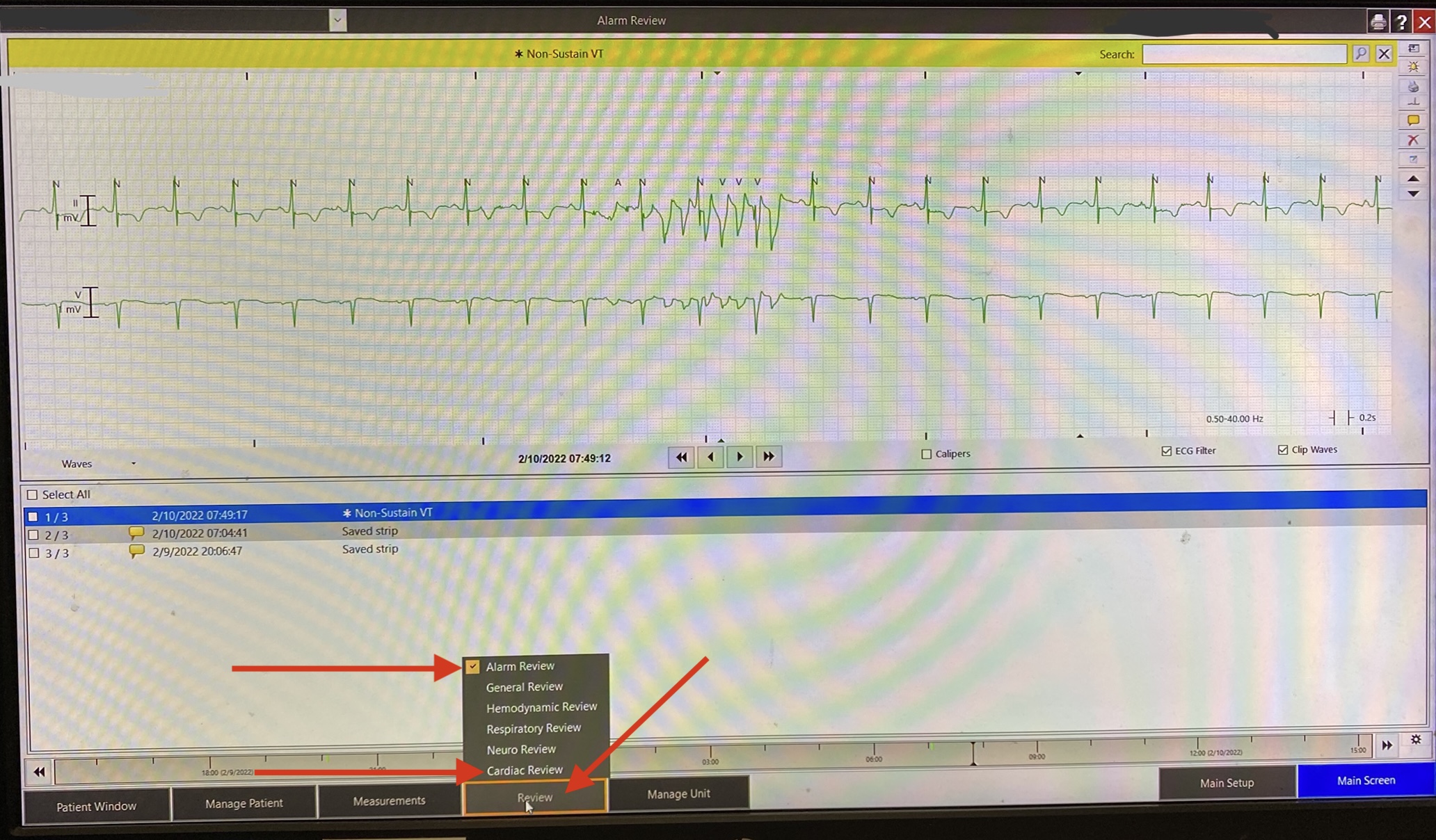
Figure 5
2- Do the tabular view (Red arrow figure 6) from the pop-up menu (Blue arrow figure 6) and change to red alarms (Red arrow figure 7) from the pop-up menu (Blue arrow figure 7).
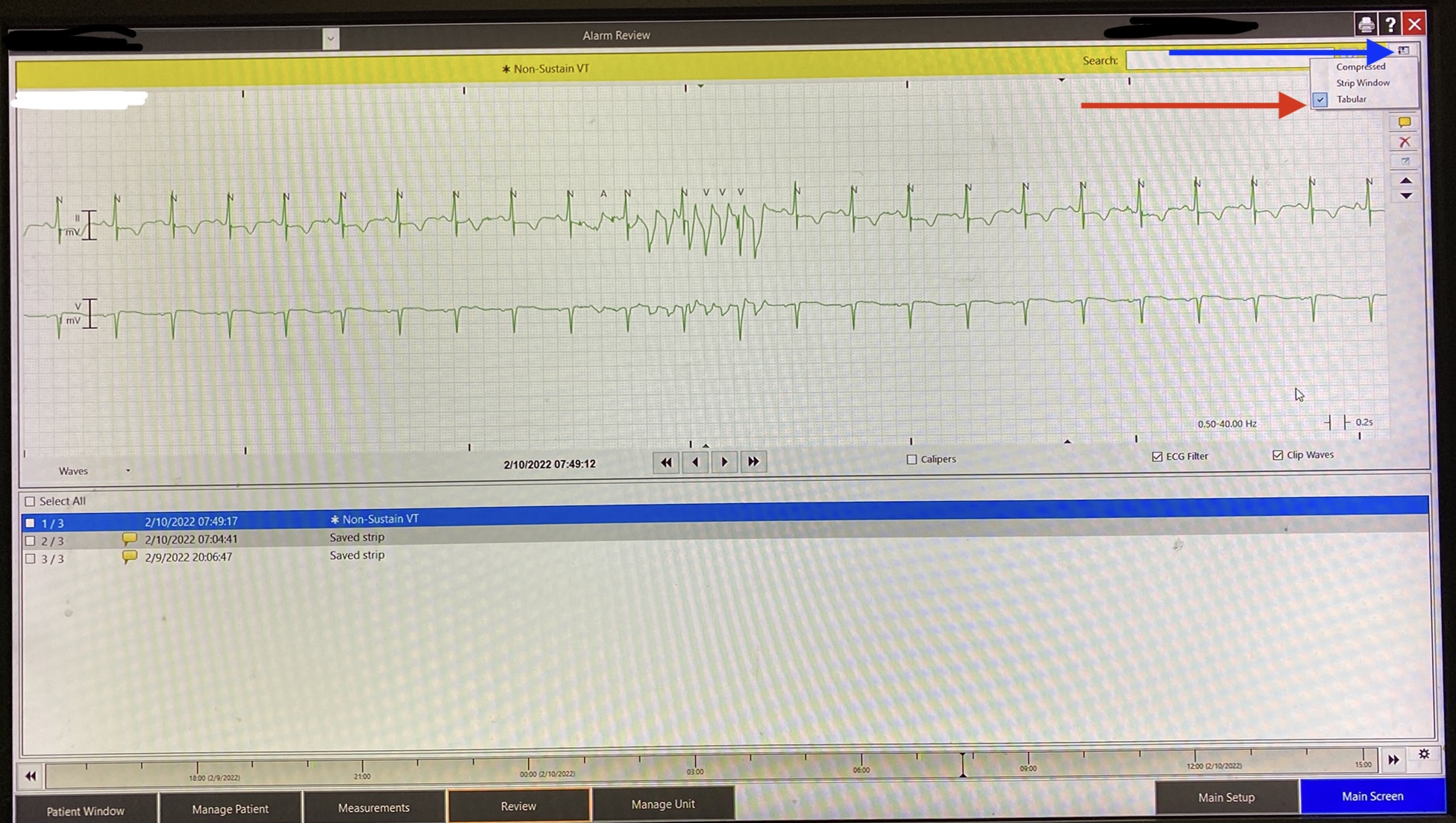
Figure 6
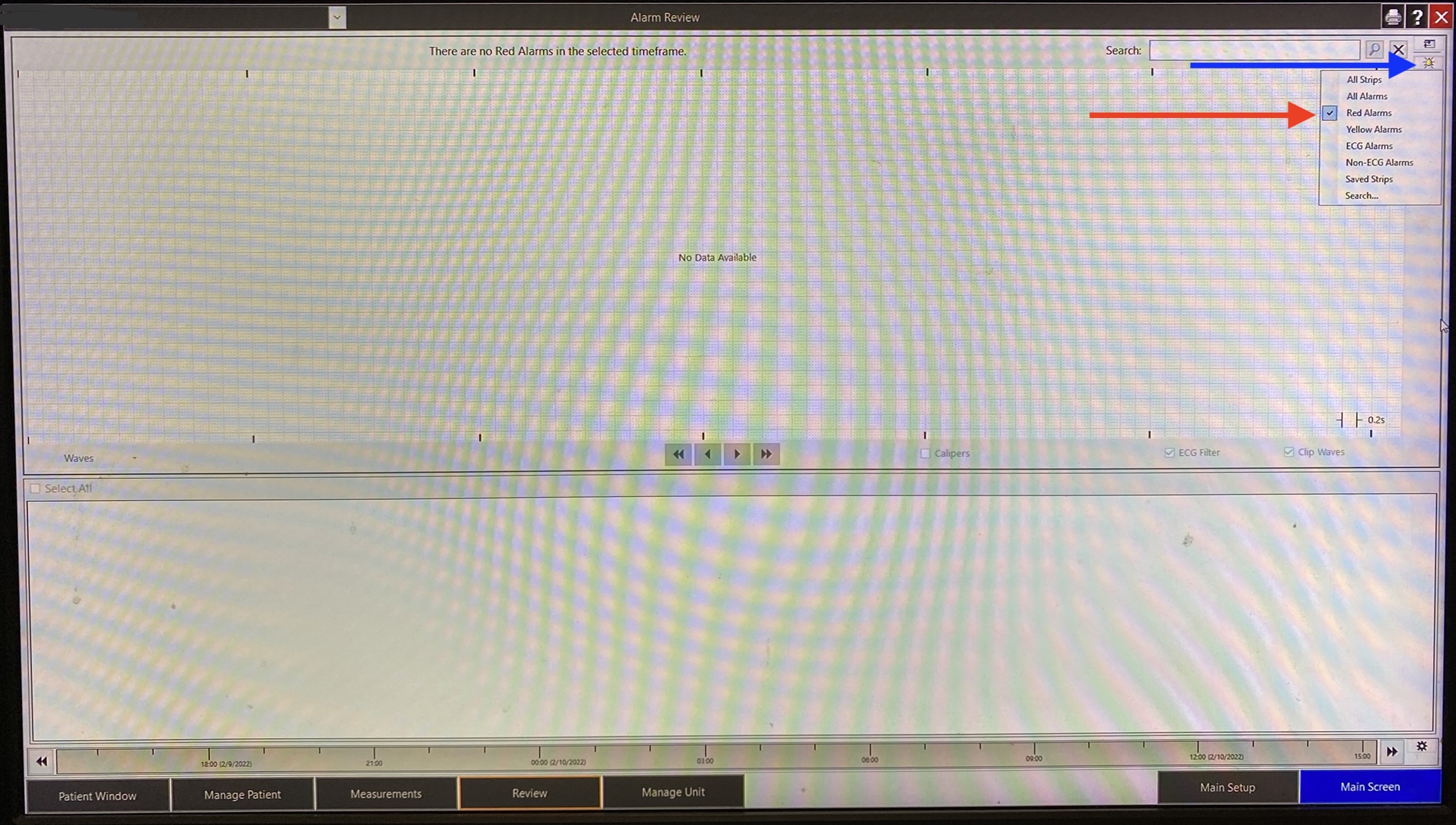
Figure 7
3- Note down the time of serious red alarms (figure 8).
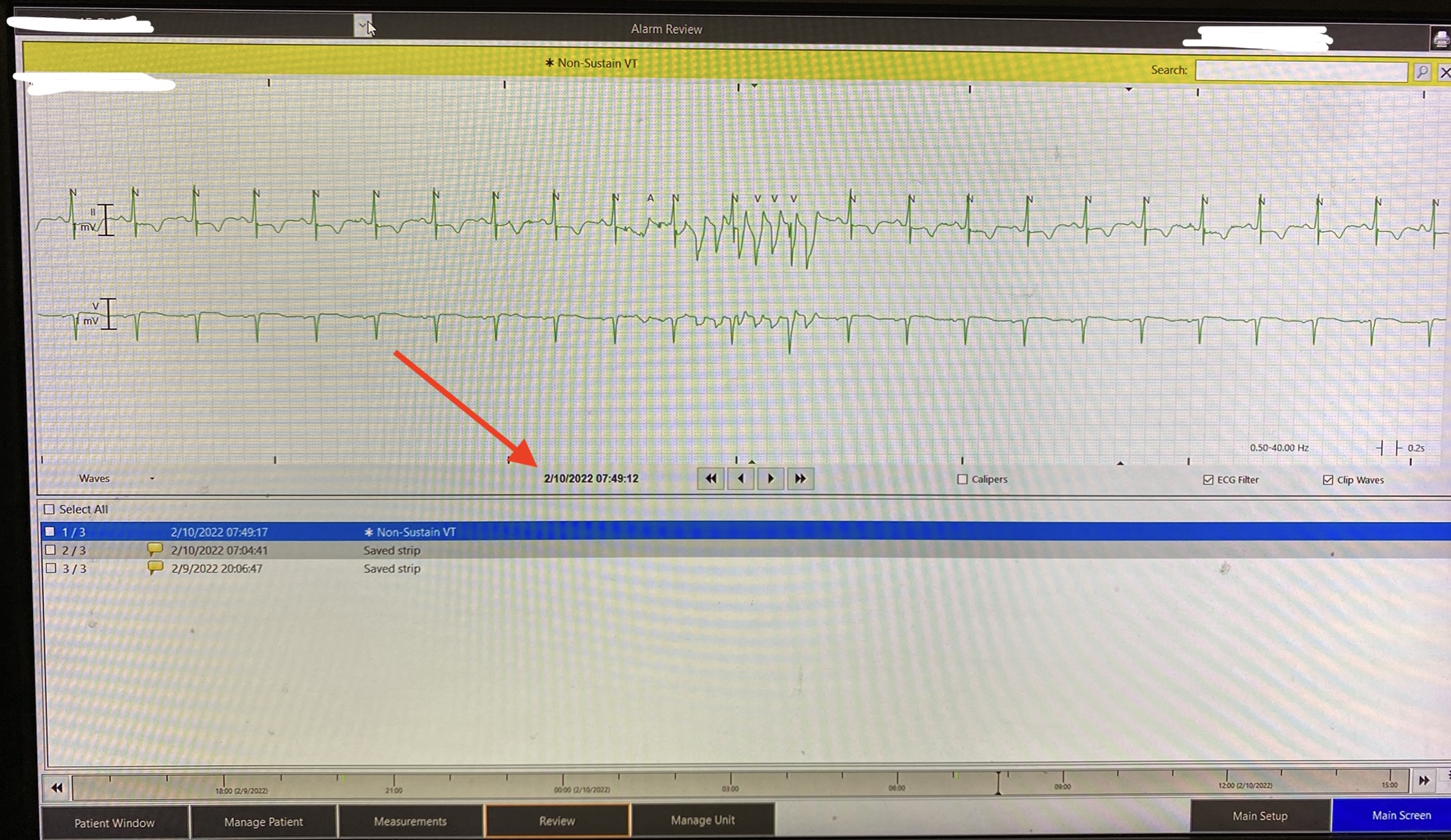
Figure 8
4- Change back to “All alarms” now and quickly scan and verify what might look serious.
5- Change to “Cardiac review” from the review tab again (figure 5).
6- Check the heart rate pattern. You can expect tachycardias such as SVT, A.Flutter, VT to show a sharp rise in heart rate compared to a gradual rise in sinus tachycardia (figure 9). This is specifically helpful when you are wondering if a tachycardia at a rate of 150 is sinus tachycardia or new-onset atrial flutter. The timings you noted from step 3 are helpful here so you can identify the onset of the tachycardia you saw in the red alarms table.
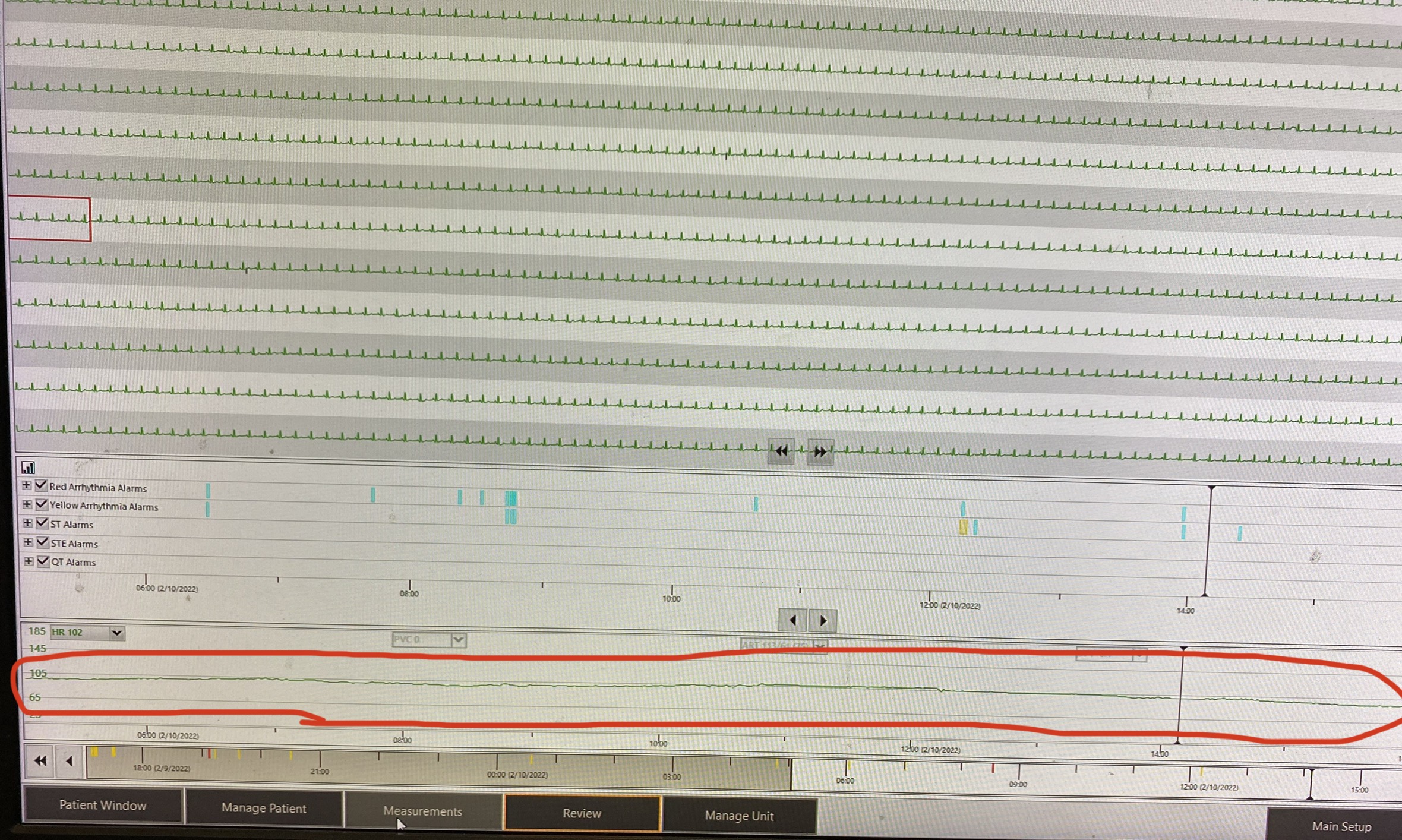
Figure 9: Notice how the heart rate has been stable in this example. It would have been gradually rising if sinus tachycardia gets worse to a rate of 140 compared to a sharp rise if the rhythm changed to atrial flutter at a rate of 140 bpm.
7- When in doubt about intervals, click on the checkbox next to “calipers”, now you can click any point on the screen and drag to measure the interval between 2 points (figure 10).
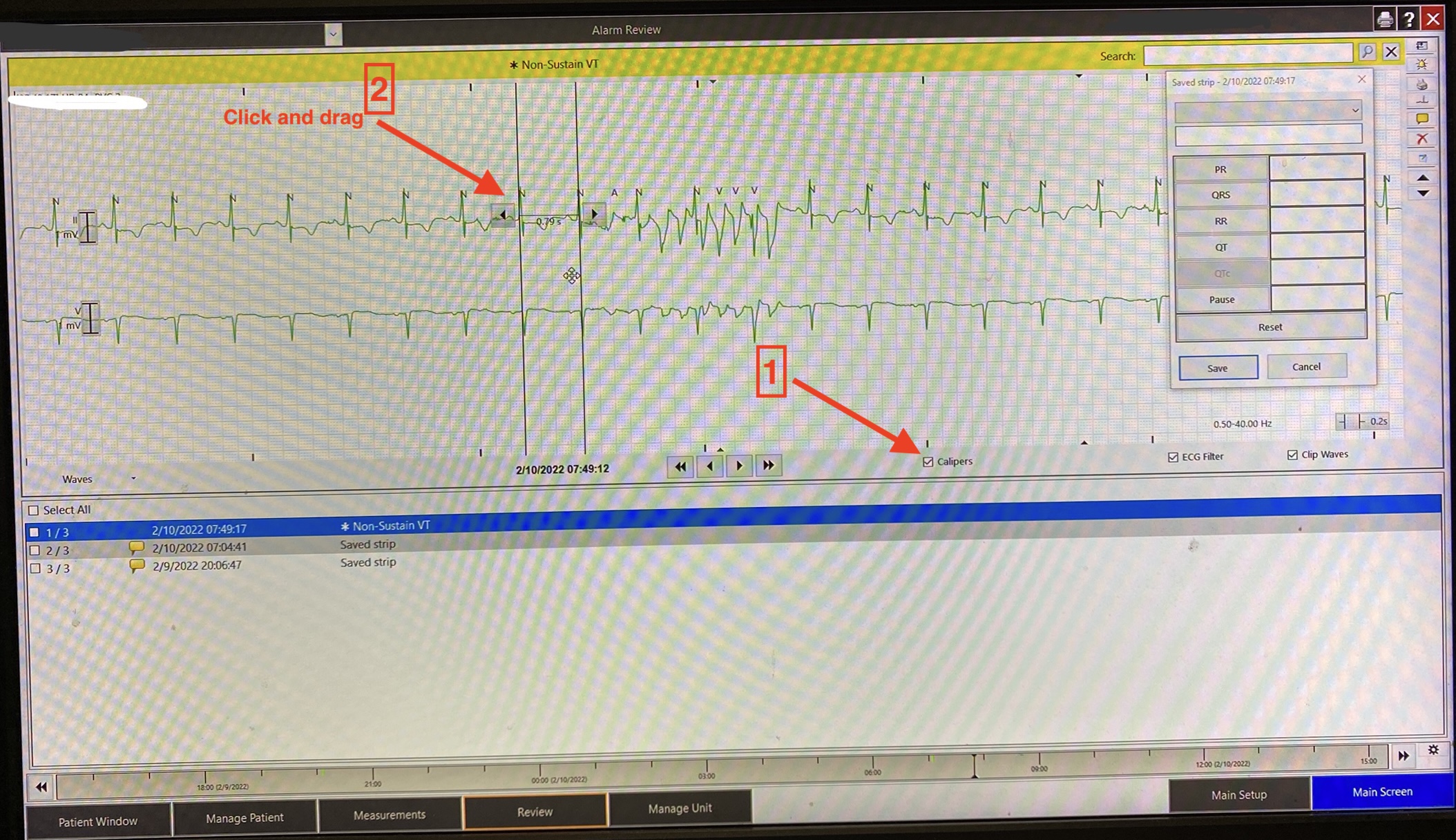
Figure 10
8- You can also march the drawn caliper by clicking on the arrow on either side to move it by the exact same interval to either side. This is especially helpful when trying to spot normal beats interspersed between artifact waves where you see sharp spikes exactly where a normal beat is expected (figure11).
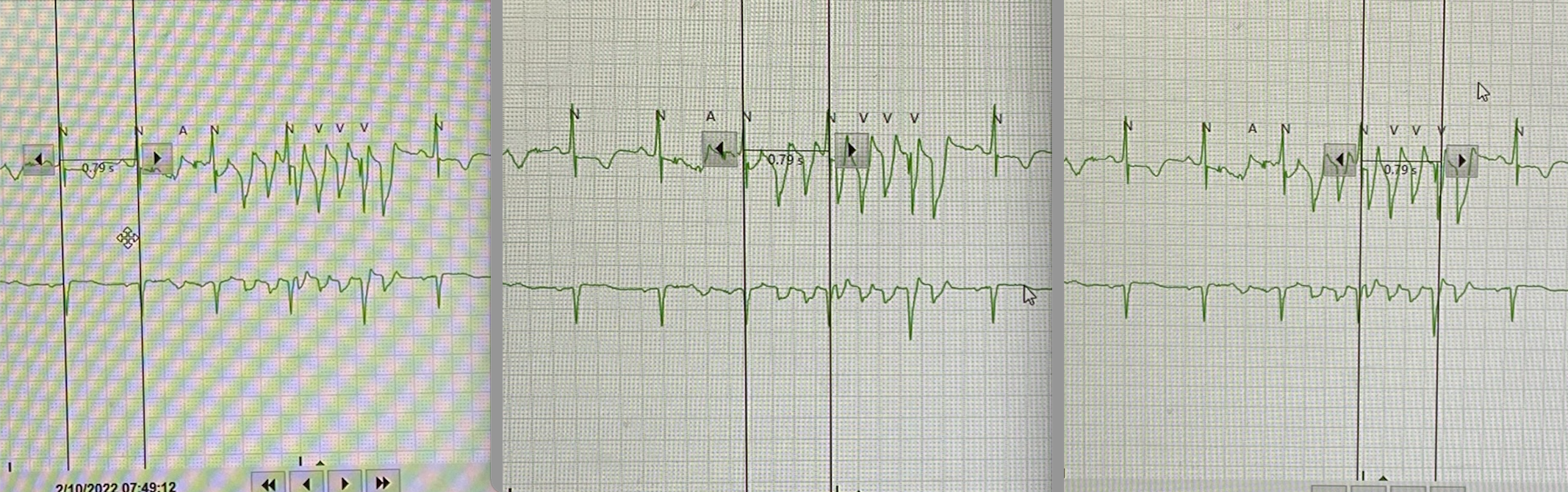
Figure 11
9- When in doubt, obtain more data by adding more leads to your screen (Arrow in figure 12)
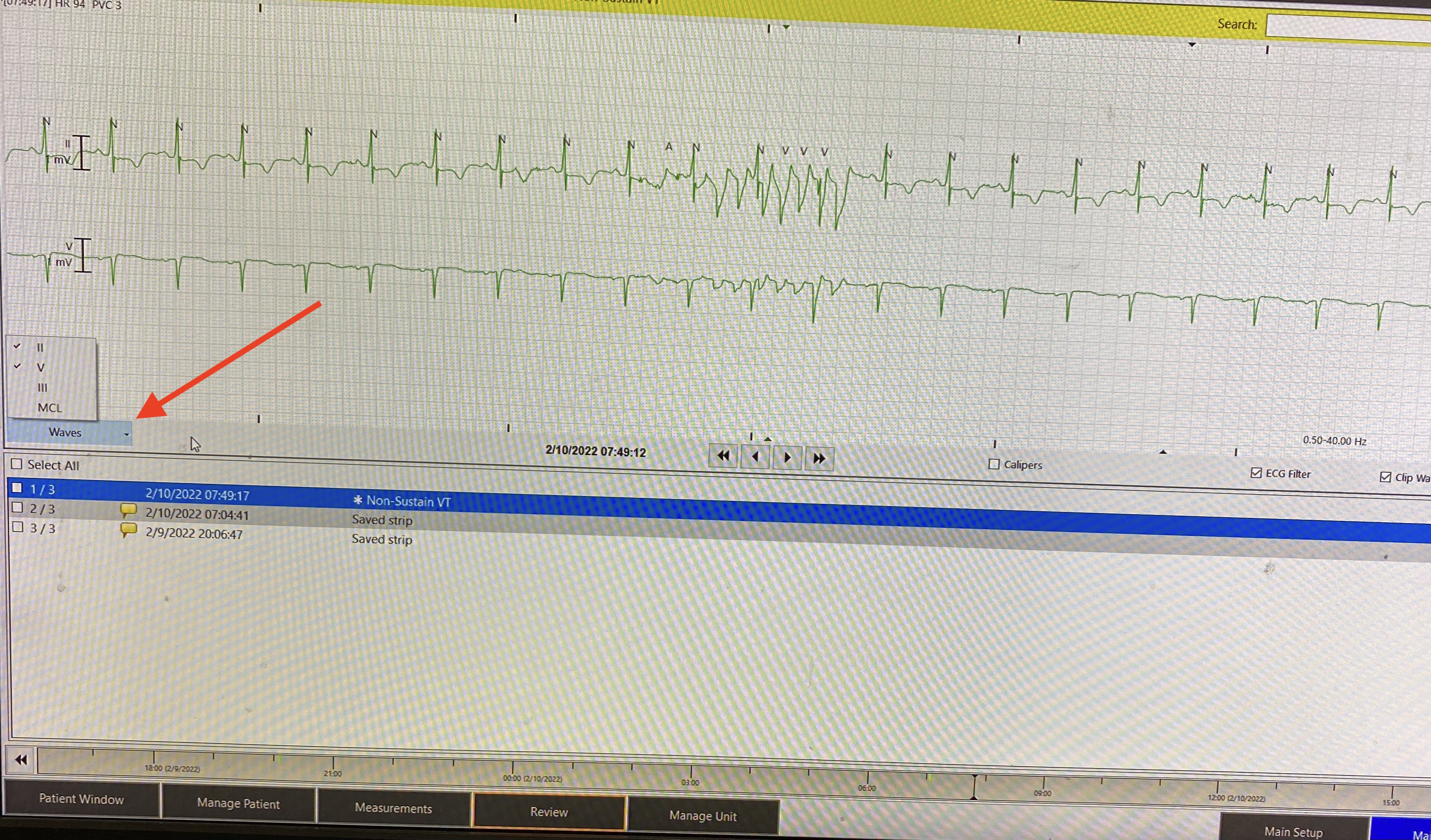
Figure 12
Bonus trick
Did you know that you can review telemetry from any unit from a single telemetry station on any floor?
1- Head over to any telemetry unit and click “review” on any of the patients in that unit (Figure 13).
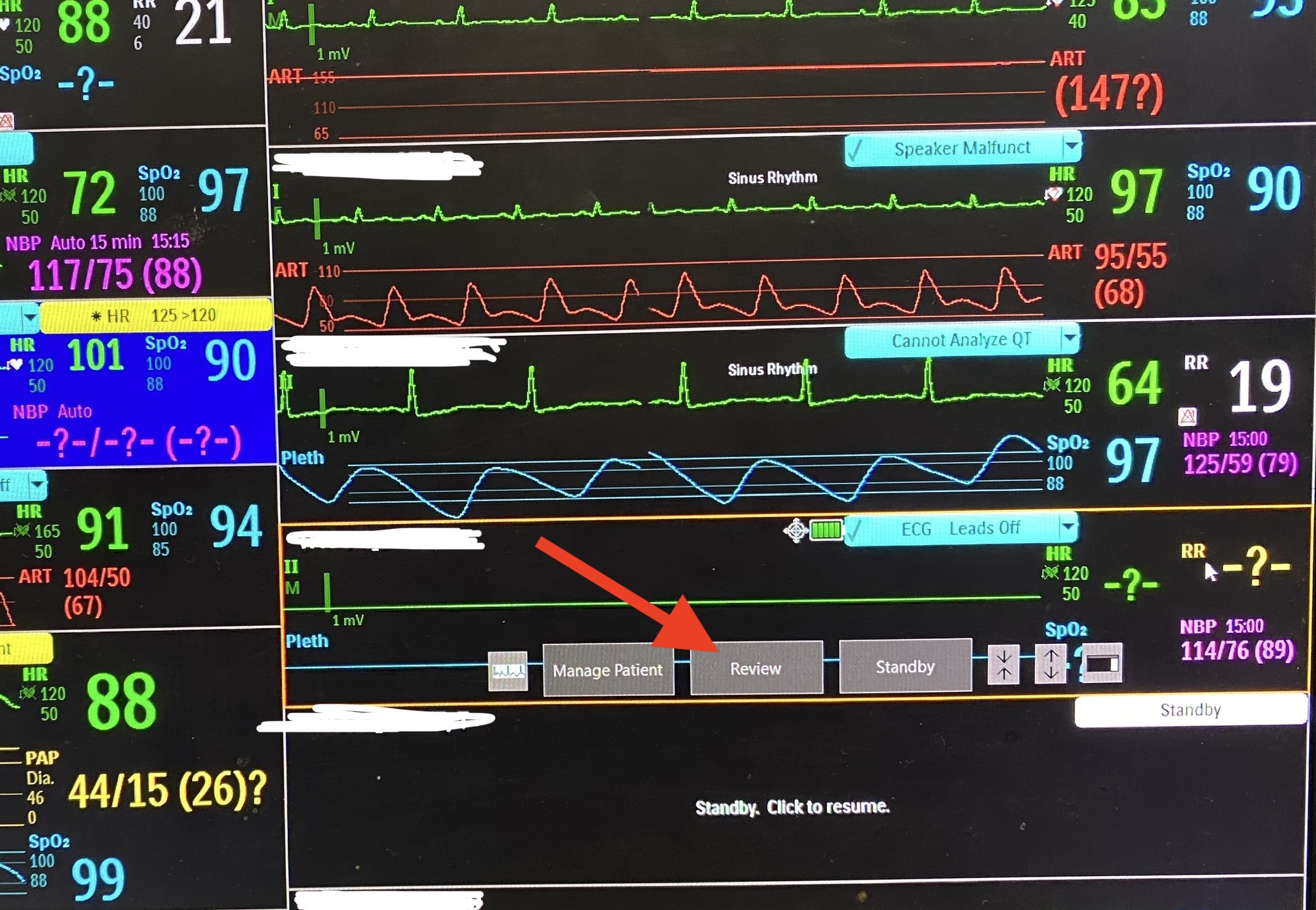
Figure 13
2- Click on the drop-down list at the top of the screen next to the patient name( Figure 14), choose the unit you want from the left pane to open all its patients in the right pane then click the patient you want to review.
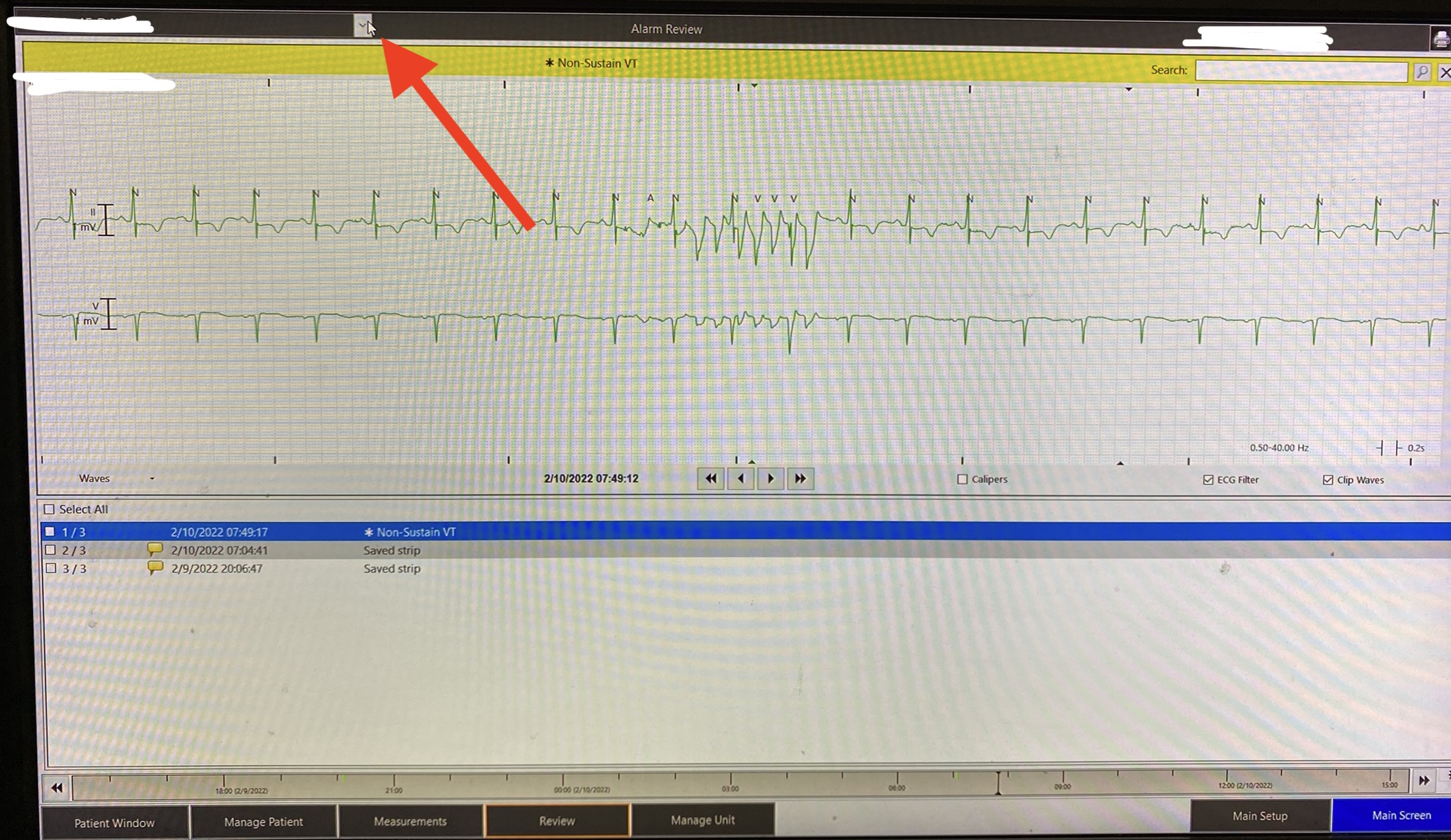
Figure 14
Now that you have (probably) learned something new, what do you think of this rhythm?
References:
- Etienne, C. "Clinical approach to arrhythmias." 40th World Small Animal Veterinary Association Congress, Bangkok, Thailand, 15-18 May, 2015. Proceedings book. World Small Animal Veterinary Association, 2015.
- Robert Buttner and Emre Aslanger. Life in the fast lane. https://litfl.com/ecg-case-137/